No country for old practices
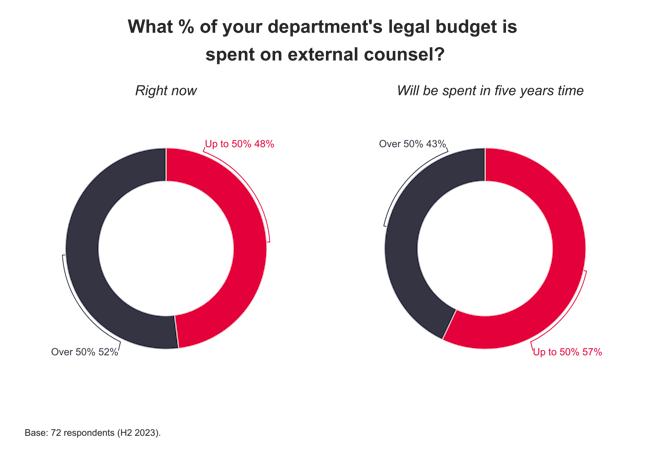
Partners may have to get used to taking a lower share of profits as firms feel the funding squeeze Firms are being squeezed on all sides. While there is pressure on fees and rising costs such as salaries, property and technology, firms are also facing funding challenges. Borrowing costs are high, few partners wish […]